Breast Reconstruction & Revision in NYC
What is Breast Reconstruction & Revision?
Restore your shape, rebuild confidence, and reclaim comfort after mastectomy, lumpectomy, or unsatisfying prior surgery. Our New York City practice offers Breast Reconstruction and Revision Breast Reconstruction tailored to your body, diagnosis, and goals—using state‑of‑the‑art microsurgery, implant‑based techniques, or a hybrid approach.
We specialize in DIEP and other perforator flaps (autologous tissue), pre‑pectoral implant reconstruction, and complex revision cases including capsular contracture, implant malposition, radiation‑related changes, and symmetry adjustments.
Breast Reconstruction restores breast shape and symmetry after mastectomy, lumpectomy, congenital conditions, or trauma. You can reconstruct with your own tissue (autologous flap), breast implants, or a hybrid of both. Timing can be immediate (during the cancer surgery), delayed‑immediate (after a temporary expander), or delayed (months/years later). Your best path depends on cancer treatment plan, radiation, anatomy, health, and aesthetic goals.
Table of Contents
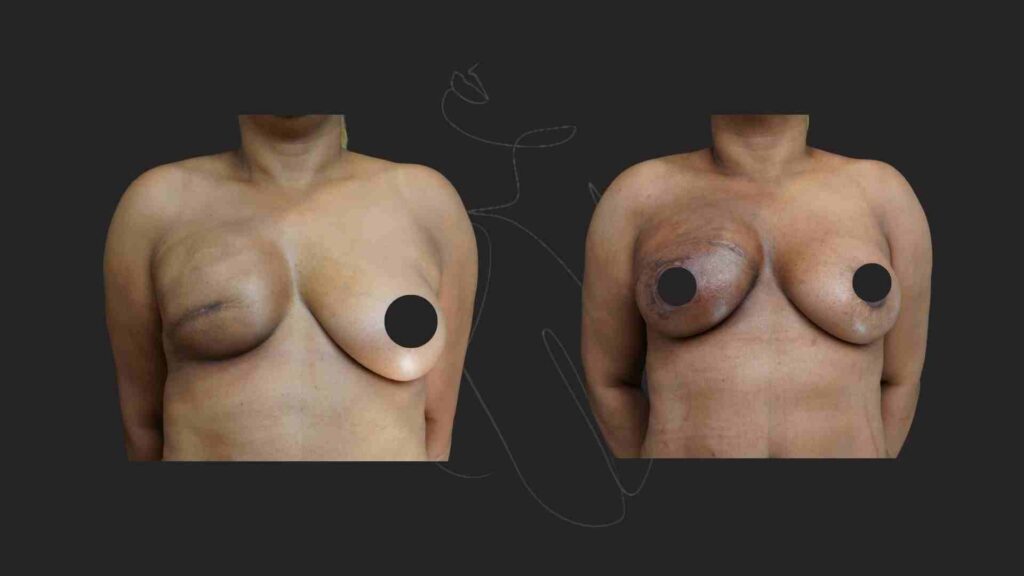
Breast Reconstruction & Revision: Before & After

Why Patients Trust Dr. Wiser
Chief of Plastic Surgery at Mount Sinai Elmhurst
Thousands of successful
procedures
Advanced techniques for natural-looking results

About dr wiser
Dr. Itay Wiser is a highly respected plastic surgeon in NYC, known for his expertise in breast surgery, mommy makeovers, tummy tucks, liposuction, and facelifts. As the Chief of Plastic and Reconstructive Surgery at Mount Sinai Elmhurst Hospital, he combines advanced medical knowledge with an artistic approach to deliver natural, long-lasting results.
With extensive training in aesthetic and reconstructive breast surgery at Lenox Hill Hospital and a fellowship in lymphedema surgery at Memorial Sloan Kettering Cancer Center, Dr. Wiser stays at the forefront of modern plastic surgery. His PhD in epidemiology and public health ensures that every treatment is backed by the latest research and techniques.
DOES INSURANCE COVER Breast Reconstruction & Revision?

Many patients wonder: “Will my insurance cover Breast Reconstruction & Revision surgery?” The answer depends on your specific plan and whether the procedure is considered medically necessary.
At WiserMD our team helps patients every step of the way — from verifying your insurance benefits to submitting the required medical documentation. We work with most major commercial insurance providers and also offer self-pay and financing options.
The only way to confirm coverage is to contact your insurance company.
At WiserMD, our experienced coordinators can assist by:
Contacting your insurance provider directly
Submitting medical records and photographs
Explaining your symptoms and history of conservative treatments
Who is a Good Candidate for Breast Reconstruction & Revision?
If you are considering breast reconstruction or revision breast reconstruction in New York City, you may be a suitable candidate if the following apply:
Mastectomy or Lumpectomy History: You are planning to undergo or have already had a mastectomy or lumpectomy and want to restore natural breast shape and contour.
Good Overall Health: You are in stable health with adequate blood supply, making you a strong candidate for safe healing after surgery.
Non‑Smoker or Willing to Quit: Non‑smokers, or patients committed to quitting smoking before and after surgery, generally experience improved recovery and reduced complication risks.
Realistic Goals: You have clear, realistic expectations about what breast reconstruction or revision surgery can achieve, whether through autologous tissue (flap) or implant-based methods.
Stable Weight: A consistent body weight enhances the predictability of outcomes and ensures long-lasting results.
Preference for Technique: Patients who prefer a natural look and feel with autologous (flap) breast reconstruction or those seeking a less invasive implant-based reconstruction may be ideal candidates.
By meeting these criteria, patients in NYC can work with Dr. Itay Wiser to create a personalized plan that restores breast symmetry, enhances body confidence, and achieves long-term satisfaction.
Technique | Key Features | Benefits | Considerations |
|---|---|---|---|
Autologous (Flap) Reconstruction | Uses your own tissue (abdomen, thigh, back, buttocks) | Most natural look/feel, durable, no implant maintenance, donor-site contouring, preferred for radiated tissues | Longer surgery/recovery, donor-site scar |
Implant-Based Reconstruction | Uses silicone or saline implants (direct-to-implant or staged) | Shorter surgery, no donor-site surgery, predictable sizing, symmetry control | Capsular contracture, rippling, rupture, less ideal with radiation, possible future revisions |
Hybrid Reconstruction | Combines flap tissue + implant | Natural-feeling coverage with precise sizing, better softness than implant-only, shorter recovery than large flap-only | Requires both implant and flap surgery, multiple techniques may increase complexity |
Autologous (Flap) Breast Reconstruction
Uses your own skin/fat (and sometimes a small muscle segment) from a donor site to rebuild a warm, soft breast mound with natural ptosis and long‑term stability.
Common Flaps We Offer:
DIEP flap (Deep Inferior Epigastric Perforator) – Low‑abdomen skin/fat; preserves abdominal muscle; gold‑standard for natural feel and long‑term durability.
SIEA flap (Superficial Inferior Epigastric Artery) – Lower abdomen tissue using superficial vessels; muscle‑sparing option for select anatomies.
PAP flap (Profunda Artery Perforator) – Posterior/medial thigh tissue; excellent when abdomen is unavailable.
TUG/DUG flap (Transverse Upper Gracilis / Diagonal Upper Gracilis) – Inner‑thigh tissue; includes small portion of gracilis muscle to achieve volume.
LAP flap (Lumbar Artery Perforator) – Flank/lower‑back tissue; helpful for abdominally thin patients.
SGAP/IGAP flap (Superior/Inferior Gluteal Artery Perforator) – Buttock tissue; preserves gluteal muscles; alternative when other sites are unsuitable.
Latissimus dorsi flap – Back tissue; often combined with an implant or fat grafting for added volume.
TdAP / ICAP flaps (Thoracodorsal / Intercostal Artery Perforator) – Back/chest wall perforator flaps for refinement and coverage.
Benefits of Flap Reconstruction
Choosing flap breast reconstruction offers several advantages for patients seeking a natural and long-lasting outcome after mastectomy or lumpectomy:
Most Natural Look and Feel: Because flap reconstruction uses your own tissue, the reconstructed breast looks and feels more like natural breast tissue, adapting as your body changes over time.
Durable, Long-Term Results: Unlike implants, flap reconstruction does not require maintenance for rupture or replacement, making it a long-lasting solution.
Donor-Site Contouring Benefits: Tissue is often taken from areas such as the abdomen, thighs, or back. Many patients enjoy the added benefit of improved contouring at the donor site (for example, a flatter abdomen or slimmer thigh).
Ideal for Radiated Tissue: Patients who have undergone radiation often achieve better outcomes with flap reconstruction compared to implant-based methods, as autologous tissue tolerates radiation effects more effectively.
Considerations for Flap Breast Reconstruction
While flap breast reconstruction provides natural and durable results, it is important to consider the following:
Longer Surgery & Recovery: Flap procedures are more complex and require longer operative times compared to implant-based reconstruction. Recovery may also be more extensive.
Donor-Site Scars & Healing: Harvesting tissue creates scars at the donor site (abdomen, thigh, or back) that require healing. These scars typically fade over time but remain permanent.
By carefully weighing the benefits and considerations, patients in New York City can make an informed choice about whether flap breast reconstruction is the best option for their personal and medical needs.
Implant‑Based Breast Reconstruction in NYC
Implant‑based breast reconstruction uses silicone or saline implants to restore breast volume and shape after mastectomy or lumpectomy. This technique is one of the most common options for women in New York City seeking a faster recovery and predictable sizing.
Approaches to Implant‑Based Reconstruction
Direct‑to‑Implant (One‑Stage): Placement of the implant immediately after mastectomy. Suitable for patients with sufficient skin and soft tissue, offering fewer surgeries and quicker results.
Two‑Stage (Tissue Expander → Implant): Involves inserting a tissue expander first to gradually create space. Later, the expander is replaced with a permanent implant.
Pre‑pectoral vs. Sub‑pectoral Placement: Implants can be positioned above the chest muscle (pre‑pectoral) to reduce animation deformity and pain, or under the muscle (sub‑pectoral) for additional support and tissue coverage.
Acellular Dermal Matrix (ADM): A supportive mesh often used in conjunction with implants to improve pocket stability and control implant position.
Benefits of Implant‑Based Reconstruction
- Shorter surgical time compared with flap procedures
No donor‑site surgery required
Predictable implant sizing for symmetry and balance
Can be performed immediately or in stages depending on patient needs
Considerations for Implant‑Based Reconstruction
Risk of capsular contracture, implant rippling, rupture, or malposition
May not be ideal for patients who have had or require radiation therapy
Possible need for revision or replacement over time
Hybrid Breast Reconstruction in NYC
Hybrid breast reconstruction combines the benefits of autologous tissue flaps with implants, offering patients in Manhattan a balanced option that maximizes softness and volume.
This method uses a flap for soft‑tissue coverage and an implant for projection or additional volume. Common techniques include DIEP flap + implant or Latissimus dorsi flap + implant.
Hybrid breast reconstruction combines the benefits of autologous tissue flaps with implants, offering patients in Manhattan a balanced option that maximizes softness and volume.
Provides a natural‑feeling envelope while achieving precise breast size
Improves softness and shape compared to implants alone
May shorten recovery compared with large flap‑only procedures
Useful for patients without enough tissue for full autologous reconstruction
Combines a flap for soft‑tissue coverage with an implant for additional volume or projection (e.g., DIEP + implant, Latissimus + implant). Ideal when autologous volume is limited or when maximizing aesthetic control is a priority.
Benefits
Natural envelope with precise sizing
May shorten recovery compared with larger flaps while improving softness vs implants alone
Is Breast Reconstruction & Revision Surgery Painful?
Most patients experience mild to moderate discomfort in the first few days following surgery, but this is easily managed with prescribed pain medication.
To further minimize post-operative pain, Dr. Itay Wiser utilizes an advanced nerve block technique during surgery. This temporarily numbs the surgical area, significantly reducing discomfort for the first 24-48 hours after the procedure. Patients who receive a nerve block often report a smoother, more comfortable recovery with less reliance on pain medication.
📌 Dr. Wiser’s focus on patient comfort ensures that you experience the easiest and most pain-free recovery possible.
Revision Breast Reconstruction in NYC
Even well‑performed reconstructions may evolve with time, weight change, pregnancy, or radiation. If your prior results no longer match your goals—or if you’ve experienced complications—we offer Revision Breast Reconstruction to restore comfort, shape, and symmetry.
Common Reasons for Revision
Capsular contracture, implant rupture/deflation, rippling, animation deformity
Implant malposition (high/low/lateral), symmastia (“uniboob”)
Radiation‑related fibrosis or contour irregularities
Flap volume loss, fat necrosis, or asymmetry
Nipple/areola position or projection concerns
Scar revision; donor‑site contouring
Revision Options
Implant exchange (size/profile/shape), pocket change (pre‑pectoral ↔ sub‑pectoral), ADM reinforcement
Conversion to autologous flap (e.g., DIEP, PAP, LAP, SGAP) for a more natural result
Hybrid revision (flap + implant) to optimize softness and projection
Autologous fat grafting to refine edges, soften radiation changes, or correct rippling
Symmetry procedures on the opposite breast: lift (mastopexy), reduction, or augmentation
Your Revision Plan A meticulous analysis of skin quality, implant pocket, radiation history, and donor‑site options informs a phased plan that sets realistic milestones and timelines.
Recovery After Breast Reconstruction & Revision
Early (1–2 weeks)
2–6 weeks
3–6 months
FAQ about Breast Reconstruction & Revision
Is breast reconstruction painful?
You’ll have postoperative soreness, managed with medications and recovery protocols. Most patients describe discomfort as manageable and improving within days to weeks.
How many appointments will I need?
Expect a preop consultation, imaging if needed, pre‑surgical visit, surgery day, and several follow‑ups in the first 6–12 weeks; additional visits for staged procedures or refinements
Can I combine reconstruction with other procedures?
Yes. Options include nipple reconstruction/tattoo, fat grafting, opposite‑breast symmetry procedures, and scar revisions. Onco‑plastic reductions/lifts can be coordinated with lumpectomy.
What if I had radiation?
Autologous flaps or hybrid approaches are often preferred to improve soft‑tissue quality in radiated fields; implant‑only recon may carry higher capsular contracture risk.
Will I have scars?
Yes, but we plan incisions for concealment and provide scar‑care protocols. Flap donor sites (abdomen/thigh/back) also have scars that fade over time.
Is nipple sensation preserved?
After mastectomy, native nipple sensation is commonly reduced; techniques like nerve coaptation are evolving but not always feasible. Nipple reconstruction/tattoo provides aesthetic restoration.
Is Revision Breast Reconstruction covered by insurance?
Often yes—especially for capsular contracture, rupture, pain, or symmetry procedures related to mastectomy reconstruction. Policy details vary.

